Share This Story
Preventing hospital-acquired infections (HAIs) isn’t just about compliance—it’s about saving lives and protecting a facility’s bottom line. Every day, 1 in 31 patients contracts an HAI, compromising safety and driving up costs.
Upgrading building systems to combat viral transmission is a smart decision with a tangible and rapid return on capital investment. By embracing advanced HVAC systems, proactive water management and intelligent automation, healthcare administrators can cultivate adaptable, longer-lasting environments—without sacrificing efficiency or sustainability.
First, Build Safe
Construction activities introduce new contaminants into hospitals, making temporary safeguards essential. Phased project implementation, isolation barriers, sticky mats, filters and pressurization controls help contain dust and pathogens, while separate pathways for workers and materials further offset germ spread.
Breathing Clean with Defensive HVACs
Airborne transmission is the leading cause of infection, making well-designed HVAC systems critical for patient health. Although the Facilities Guidelines Institute (FGI) and ASHRAE set baseline system standards, many care networks are going beyond these requirements, adopting next-generation approaches to bolster indoor air quality.
Optimizing Air & Ventilation
The 2014 FGI Guidelines decreased minimum air changes per hour (ACH) in patient rooms from 6 to 4, improving energy efficiency but slowing airborne contaminant removal. To compensate, many organizations have increased ACH to 8 or 10 to accelerate the purification process. Computational fluid dynamics (CFD) and displacement ventilation further augment airflow, eliminating dead zones and balancing energy efficiency with cleanliness.
At the height of COVID-19, hospitals also increased outdoor air ventilation rates to help stop the spread, but at a steep energy cost. Now, web-based digital controls offer a smarter option, modulating intake in real time to harmonize air quality and energy conservation. These systems can even activate emergency modes, maximizing fresh air and exhaust during outbreaks.

At Wayne Memorial Hospital, new air handling units (AHUs) deliver 20 ACH during surgeries, then automatically scale down to save power.
Air quality monitoring platforms can also track particulates, CO₂ and volatile organic compounds for automated HVAC system adjustments. Collected analytics help elevate airflow, prevent contamination spikes and detect pathogens early, promoting purity in vital spaces.
Filtration for Pathogen Neutralization
Not all air filters are created equal. The Minimum Efficiency Reporting Value (MERV) rating classifies filters based on their ability to trap particles, with higher levels offering more robust filtration. The strongest include:
- MERV-13: Captures mold, dust and common allergens
- MERV-14: Traps bacteria and respiratory droplets
- MERV-16: Near-HEPA-level protection, ideal for procedure rooms
High-Efficiency Particulate Air (HEPA) filters remove 99.97% of particles as small as 0.3 microns but demand massive energy loads to function. Additionally, integrating Ultraviolet Germicidal Irradiation (UVGI) within AHUs neutralizes pathogens before recirculation, prevents biological growth on cooling coils and saves fan energy while refining air quality.
Humidity Control
Relative humidity below 30% prolongs airborne virus survival, increasing transmission exposure, while levels above 60% foster mold and bacterial growth, leading to secondary ailments.
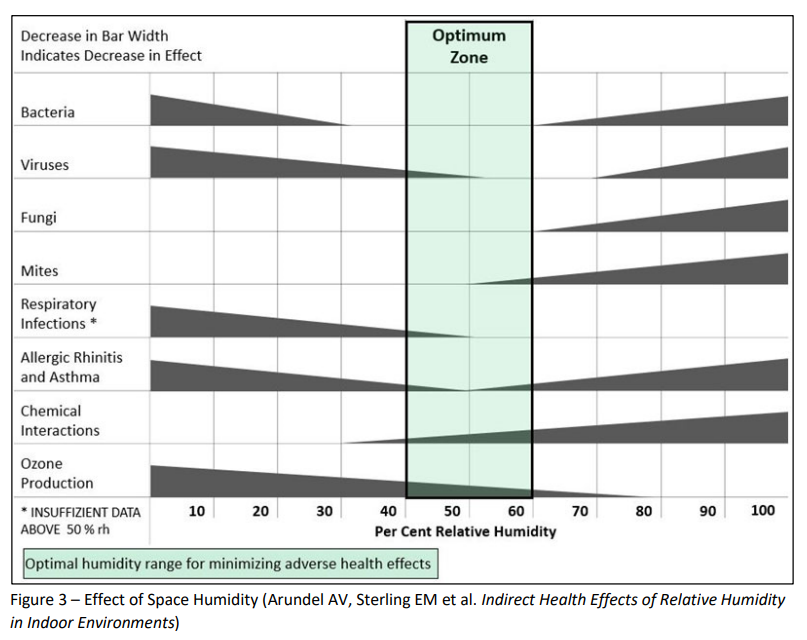
Facilities can achieve a delicate balance by installing desiccant dehumidifiers in sterile spaces, alongside steam or adiabatic humidification for consistent dew point control.
Mitigating Waterborne Hazards with Progressive Plumbing
While airborne pathogens dominate infection control discussions, waterborne illnesses like Legionella pose equally severe threats. Forward-thinking water management—not reactive intervention—is key to proper hygiene.
- Storing Hot Water at 140°F: Legionella thrives in stagnant, lukewarm water (~100°F), but hospitals can store water at a higher temperature and mix it down to 120°F for distribution.
- Water Management Program: Following CDC guidelines, hospitals can implement this with quarterly sink testing, high-heat flushing and chlorination to stop outbreaks before they start.
- Hands-Free Fixtures: Touchless laminar flow faucets, sensor-activated doors and auto-flush toilets minimize surface contact, and copper-alloy and antimicrobial plumbing materials fight bacteria.
- Reduced Pressure Backflow Preventers (RPBPs): By maintaining a consistent pressure differential, these devices guarantee that contaminated water cannot re-enter clean systems, preserving water quality.

Chlorine dosing ports were added to Mount Nittany Medical Center’s domestic water system—in accordance with their water management program—allowing staff to isolate and disinfect piping with high-concentration chlorine if contaminants are detected.
Energizing Resilience with Advanced Electrical Systems
Infection control cannot happen without reliable power, necessary for sustaining HVAC systems and water monitoring. A single outage can jeopardize these protections, increasing viral hazards.
To get ahead, hospitals must integrate redundant power sources, including uninterruptible power supply (UPS) systems for short-term ventilation backup, generators to maintain negative pressure and microgrid technology with battery storage for decentralized power.
UV-C & Smart Disinfection
Electrical and lighting systems can also play an active role in infection control. UV-C sterilization in HVAC ducts and overhead fixtures vaporizes airborne pathogens, and indigo-clean light can be used to disinfect unoccupied patient rooms.

At Holy Spirit Medical Center, UV-C and indigo-clean lighting work in tandem—green filaments enhance visual acuity during procedures, and sterilization activates post-op to kill bacteria.
The Future of Infection-Resistant Design
In the wake of a global pandemic, once-overlooked building systems have emerged as frontline defenders of physical health and wellness, shaping how hospitals tackle today’s challenges and prepare for the unknown. Healthcare leaders who invest in dynamic design don’t just stand to lower liabilities and treatment costs—they’re setting new benchmarks for durability and human-centered care for generations to come.
