The SARS-COV-2 virus pandemic has forever changed the way that facilities are constructed, operated and managed. As happens with most crises, there are currently many attempts to find a quick solution to the problem. Consequently, there is a lot of misinformation or incomplete information about what can work to control the virus. Nonetheless, it is proven that building systems, particularly the building HVAC systems, will play a significant role in potentially controlling the spread of the virus.
Earlier this year, ASHRAE published the following public policy statement regarding the transmission of the SARS-COV-2 virus:
“Transmission of SARS-CoV-2 through the air is sufficiently likely and airborne exposure to the virus should be controlled. Changes to building operations, including the operation of heating, ventilating, and air- conditioning systems, can reduce airborne exposures.”
In line with this statement, research and operational procedures have identified four basic areas of emphasis that should be addressed by building HVAC systems: Ventilation, Filtration, Decontamination, and Space Temperature and Humidity Control.
Ventilation
Increasing the amount of outside air ventilation has been one of the most publicly talked about solutions to the coronavirus problem in building systems. It is true that increasing the amount of outside air in a building, and minimizing the amount of air that is recirculated in the building, can help dilute airborne pathogens. In turn, it has been widely suggested that all HVAC systems should be set to provide 100% outside air.
However, there are consequences to increasing the amount of outside air being introduced into a building. The heating and cooling systems in a building may not be sized to handle the additional load imposed on the system by increased amounts of outside air. Consequently, the system may no longer be able to control the temperature and humidity in the building spaces, causing the indoor condition to become unacceptable. Even if the heating and cooling equipment could handle the additional load of the outside air, increasing the amount of outside air through any air handling system will inevitably increase the amount of energy consumed to condition that outside air, and ultimately increase the energy utility costs associated with running that equipment.
Finally, the air handling equipment in many buildings cannot be adjusted to provide 100% outside air, and many buildings still do not have a central air handling system at all. Therefore, it is necessary to evaluate each building individually to determine the most effective way to ventilate the building spaces.
Filtration
Improving the filtration of air circulating into building spaces can be an effective way to help control the spread of pathogens. To successfully do this, the filters used must be able to contain very small particles, and common, off-the-shelf filter media cannot filter particles small enough to capture the necessary pathogens.
It has been shown that filters rated as ASHRAE MERV-13 or higher, or HEPA rated filters, can be used to contain most bacteria and viruses. The MERV rating system only tests filtration of particle sizes down to 0.3 microns, and MERV 13 is the first rating size where a significant percentage of particles of that size are captured. While the SARS-COV-2 virus is about 0.12 to 0.14 microns in size, a minimum rating of MERV 13 is recommended since research has shown that at least 20%-25% of virus particles can be contained with MERV 13 filters.
Once again, however, there are consequences to increasing the level of filtration in any air handling system. MERV 13 and HEPA filters are typically larger and thicker than the more common MERV 6 or MERV 8 filters, so they may not physically fit into an existing air handling system. The increased amount and effectiveness of the filtration will also cause increases in the system resistance that a fan will need to overcome to properly circulate the air. To overcome these increases in system pressure drop, the fan horsepower will need to be increased, again causing increases in energy consumption and utility costs.
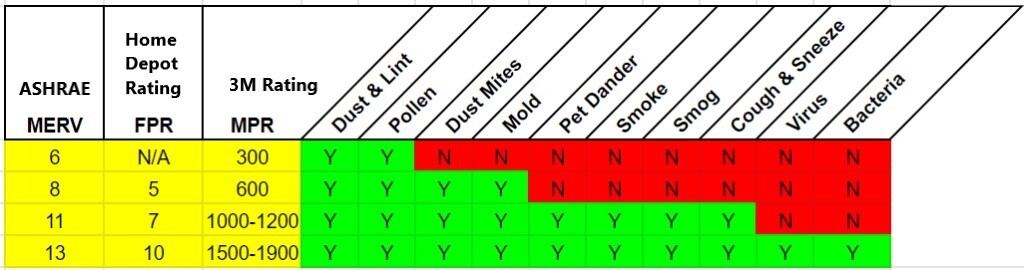
Figure 1 – Filter Efficiencies
Decontamination
Lately, there has been a lot of marketing and advertising information about the use of ultraviolet (UV) light in building systems to kill and eliminate bacteria and viruses. From this information, one might assume you could just hang a UV light in your air handling system and the virus would be controlled. The reality, however, is not quite that simple.
All UV light affects the growth of bacteria and some viruses, but the lower wavelengths of the UV-C range (200-280 nm) have been shown to be the most effective at killing the dangerous pathogens. In order to be effective, the bacteria and virus must be exposed to this UV light for a period of time – typically at least 2 minutes. Simply aiming UV lights at the airstream in ductwork or an air handling system may not be effective. Generally, the air flow through this part of any system will be moving too quickly to provide the required minimal exposure to the light.
UV light can be effective for controlling pathogens on components of an air handling system – like cooling coils, heating coils and filter banks – through surface disinfection where particles could be accumulating over a period of time. It should be noted that all UV light is potentially dangerous to humans, and safety controls must be considered when installing and operating this equipment.

Figure 2 – UV-C Light on Coil and Filter Bank
In addition to UV light, there are other decontamination technologies that are now proving to be effective at killing or controlling potential pathogens. Specific types of electronic air cleaners, and technologies such as bipolar ionization, have recently been identified as potential weapons against the spread of the SARS- COV-2 virus.
Since the research and information about these technologies is constantly changing, it is recommended that any system being considered be properly investigated. As always, each individual air handling system should be studied to determine the feasibility of any decontamination system.
Space, Temperature and Humidity Control
While it is important to control temperature and humidity levels for obvious comfort reasons, research has shown that maintaining humidity in a space between 40% and 60% significantly reduces the transmission of viruses and bacteria. In fact, there appears to be little or no transmission of pathogens through the air at humidity levels in this range. When environment humidity levels go below 40%, the transmission of airborne viruses has been shown to significantly increase, which may be one explanation for the increase in influenza cases during the winter months.
Consequently, the addition of humidification to air handling systems, or directly to inhabited spaces, should be considered in any plan to reduce viral infections. HVAC system controls should also be analyzed, modified and adjusted as necessary to maintain this optimum range of humidity during both cooling and heating seasons.
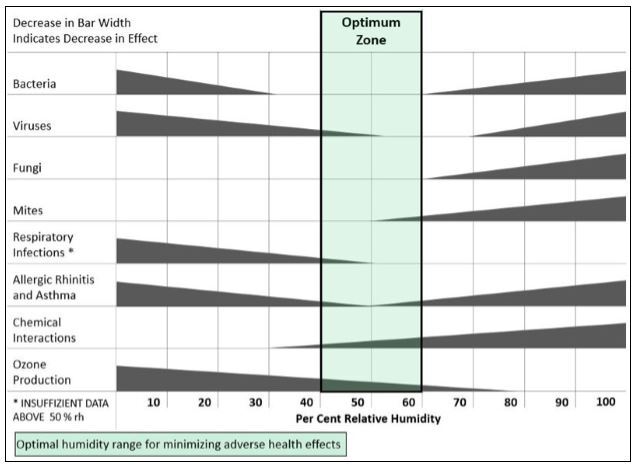
Figure 3 – Effect of Space Humidity (Arundel AV, Sterling EM et al. Indirect Health Effects of Relative Humidity in Indoor Environments)
Summary
Each of the four topics above should be addressed in building environmental systems when developing a plan for controlling the spread of pathogens in the indoor environment. It is important to have a professional review each building and its systems individually. Modifications to equipment and operating procedures can be identified within each of these areas as a part of this review. Some modifications will be easier and less expensive than others to install; and each potential change should be analyzed for practical and financial feasibility.
Additional Resources
There is a lot of information available about the coronavirus pandemic and the built environment. The Center for Disease Control, the World Health Organization, manufacturers, and numerous industry organizations have all published web pages, brochures, and other readily available material. One of the best and most complete collections of information about this issue is the web page created and maintained by ASHRAE’s Epidemic Task Force.
Please contact CPL Principal, Thomas H. Phoenix, P.E., FASHRAE, LEED AP, or CPL Vice President, Dave Hart, P.E., for more information.
